Blog
Can chronic swelling be treated?
Posted on November 17, 2019
Chronic oedema is a serious progressive medical disorder that should be treated promptly. This photo represents a typical case of of chronic swelling in the ankles and legs that have been left untreated for more than 10 years. It is probably due to longstanding incompetent leaky veins in the legs and repeated infections over time. Do you notice the discolouration, brown staining, change in skin condition (thick and dry) and overall enlargement of the legs and feet that developed? These changes makes day-to-day living challenging such as finding footwear that fits, walking and balance can become an issue.
The ‘after’ photo is the same patient’s leg after only 2 sessions within 6-weeks. There is reduced swelling and the skin looks better. The patient reported that her legs feel lighter so exercises and overall mobility has improved. Importantly, diuretics (water tablet) was not used to achieve this effect. Reach out to LK Lymphoedema Centre for a bespoke management approach suitable for you. Book an appointment online.
Should I use a compression pump? Self manage my lymphoedema?
Posted on October 27, 2019
This is a report from one of my client regarding use of her compression pump:
“I’ve had my compression pump for 12 months now and feel it is the best purchase I have made to self manage my lymphoedema. I didn’t get a health fund rebate on the actual pump but got 85% back on the leg sleeve. I am happy with what I spent when I compare that to the cost of having MLD done or even hiring the pump – it paid for itself in less than 6 months (compared to hiring).
I keep it next to my bed (with the leg sleeve and cables in a large basket) plugged in ready to go – no excuses! I do the half hour (per leg) massage 5-6 times a week wearing either a Mobiderm or Caresia garment for added benefit although it still does a good job without these. The massage it gives is quite firm but also relaxing and I either read or watch tv while its going on. I can feel it working down then up my leg similar to MLD and it works the back of my leg really well, which is a hard area to do yourself. I put my compression stockings on as soon as it is done.
As lymphoedema is a lifelong condition I accept that self management is the way to go (along with the guidance of a good therapist of course!) and this pump makes that easy to do. With continued regular use I feel my leg is a lot softer than it was and I see a marked improvement in the ankle and calf areas.”
Report on the Australia ILF-COM project
Posted on October 14, 2019
 This is a report by Dr Linda Khong as a follow-up to her participation (Australian) with the International Lymphoedema Framework- Chronic Oedema Outcome Measures (ILF-COM) project. Twelve frameworks involving 8014 people took part in the survey conducted December 2018 to end of March 2019. Each framework reported their respective ILF-COM findings via posters at the ILF Conference in Chicago 13-15 June 2019.
This is a report by Dr Linda Khong as a follow-up to her participation (Australian) with the International Lymphoedema Framework- Chronic Oedema Outcome Measures (ILF-COM) project. Twelve frameworks involving 8014 people took part in the survey conducted December 2018 to end of March 2019. Each framework reported their respective ILF-COM findings via posters at the ILF Conference in Chicago 13-15 June 2019.
Overall, the survey’s international respondents demonstrated that patients and healthcare professionals viewed limb volume, quality of life status and mobility status as three most important outcome measures as well deemed successful outcomes.
What causes chronic swelling?
Posted on October 10, 2019
There are many causes of leg swelling that is NOT due to Lymphoedema. Click here to read more about it from Mayo Clinic. Reasons for such swelling may arise from medications, being wheelchair bo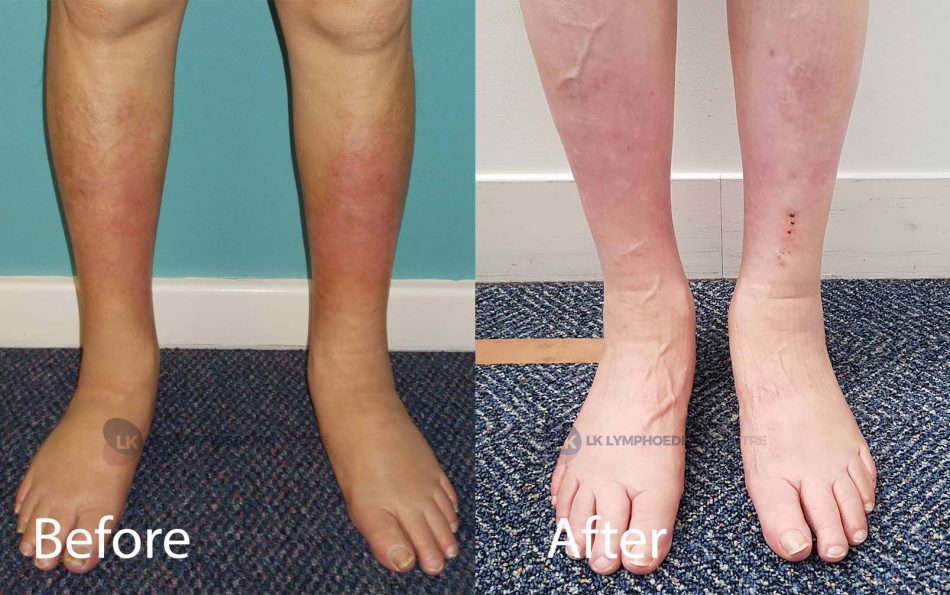 und, renal/cardiac issues and other reasons.
und, renal/cardiac issues and other reasons.
For example, this client (see photos included with permission) had persistent swelling in both legs, skin discolouration and repeated infections with skin tears a few years ago. The chronic swelling arose from several causes.
What do you think are the factors to successful effective oedema management in you case?
I have Type I diabetes and a history of renal failure with renal transplant in 2001. I have had vascular oedema of both legs for about 6 years or so. It has been exacerbated by antihypertensive (blood pressure) medications, in particular, calcium channel blockers.
The most important factor in managing my oedema has been the regular and consistent wearing of elastic stockings. Keeping on top of the swelling. This helps the swelling at bay and has improved the condition of my skin of lower limbs and no longer at risk of skin lesions and cellulitis.
Before photo was taken 1 year after regular treatment of CDT , stockings and more at the clinic.
After photo was taken 4 years later (2019). No more episodes of infections since treatment started, markedly reduced swelling and improved appearance. From the therapist’s perspective, the positive outcome can be attributed to thorough assessment cum management and the client’s positive attitude with sustained regular follow-up over time to manage the chronic condition.
It is important that you seek medical clearance first especially if you have swelling in both legs before booking an appointment with the clinic.
What is lipoedema?
Posted on September 7, 2019
Lipoedema is a chronic fat syndrome that is not well understood and sometimes misdiagnosed as Lymphoedema or it may be combined with lymphoedema. Therapy maybe similar to lymphoedema but not the same. Help is available at this clinic, click here for therapy that can be of help.
Lipoedema affects mainly women. There is usually symmetrical abnormal fat deposits at the legs involving the hips, buttocks, thighs and calf but not the feet. This looks disproportionate when compared to the upper part of the body. There may be reports of pain, tenderness and sometimes a family history, too. To learn more about lipoedema, click the following via Lipoedema Australia, Lipoedema UK, and Fat Disorders Resource Society. The West newspapers reported on Lipoedema in a recent article.
Do you look like this (in the photos)? Have you been called “Thunder thighs’ since teenage years? But your feet is fine?
An example of a client with Lipoedema (Photos included with permission). Client’s feedback “Many thanks Dr Khong for your expertise and skill in treating my lymphoedema and lipoedema. As a visitor to Perth annually having Lymphatic Manual Drainage here has enabled me to feel confident to continue to make these family trips.”
What is Lymphoedema or Lymphedema and what causes it?
Posted on June 19, 2019
This is tissue swelling caused by a defect of the lymphatic system which is a part of the immune and circulatory system. Lymphoedema can arise from primary or secondary causes.
Primary causes are congenital in origin that can manifest at different stages of life. That is, at birth, teenage or later in life commonly middle age. Do you have other family members that have similar presentations as you?
The other causes can be Secondary due to trauma; injury; surgery including removal of lymph node(s) in cancer, hip/knee replacement; vascular procedures e.g. vein stripping; radiotherapy, infection, being wheel-chair bound or simply being severely overweight.
There are other conditions that may appear to Lymphoedema, too. Once you have received medical assessment and clearance by your doctor, the clinician (Linda) can help you work out what the possible cause is and how to address the condition.
Signs and symptoms of Lymphoedema
Posted on
Lymphoedema is a form of tissue swelling that develops gradually and can present in any part of the body but more commonly in the legs.
If the condition is left unaddressed for an extended period of time, the common signs and symptoms include:
- Swelling in any part of the body e.g. legs, feet, arms, head and neck, breast
- Heaviness and restricted movement
- Delayed wound healing
- Skin thickening (fibrosis) and other skin changes or growth
- Repeated infections and sometimes hospitalisation
- Localised discomfort and pain
What is Complete Decongestive Therapy (CDT) and Compression Therapy?
Posted on June 24, 2019
Compression Decongestive Therapy (CDT) is a recommended comprehensive treatment for lymphoedema. The aim of CDT is to reduce the swelling and to prevent re-accumulation of lymphatic fluid in the body part. A critical component is application of Compression Therapy consecutively for an intensive period of time followed by a maintenance period.
Compression therapy may involve Compression Bandaging of the affected body part or Compression Wraps, Compression Stockings and/or Compression Pumps.
Working together with you, our clinician will help you in various ways. For example, to improve your capacity to walk, relieve your pain, exercise, and/or return to do what is important to you (Tell the clinician at your First Appointment).
What is Manual Lymphatic Drainage (MLD)?
Posted on June 19, 2019
MLD is a specialised massage therapy to facilitate lymphatic drainage away from the area of swelling. It is one of the integral components in the best practice treatment guidelines.
Your clinician (Linda) is fully certified as an Advanced Practitioner since 2003. She is trained in the Dr Vodder CDT and MLD technique and also with the Lymphoedema Training Academy. She will apply a specialised light stroking massage technique to help with your swelling.
What are the treatment options for lymphoedema?
Posted on
Currently, lymphoedema is an incurable and progressive chronic condition.
However, it can be managed successfully if addressed as early as possible and on a regular basis for an excellent quality of life.
This clinic offers various services that involve conservative (non-surgical) treatment options.
The main treatment highly recommended is Complete Decongestive Therapy (CDT).
This includes an intensive phase of Compression Therapy, Manual Lymphatic Drainage (MLD) and exercise.
Your clinician (Linda) will assess and tailor a suitable plan for you, if indicated.




























