News
Help! What do I do with swelling (Lymphoedema) after my Prostate Cancer?
Posted on July 1, 2023
Physiotherapist, Dr Jo Milios & Sexologist/Nurse Practitioner, Melissa Hadley Barrett based in Perth, Western Australia host The Penis Project. It is a podcast that covers topics on men’s private parts. Podcast Episode 138 from The Penis Project, titled ” Meet Brian and Vanessa – Recovery, Injections, Lymphedema, and 2-3 rounds” shares some insights on their journey dealing with the challenge. I am so proud and thank the hosts and Brian for coming forth to share such intimate details so that others can learn from his experience.
There is hope for management of lymphoedema swelling impacting on sexual function following Prostate Cancer. Do not despair, you can continue to have a quality of life, just work with your lymphoedema therapist.
Lipoedema can be painful, manageable and is NOT obesity
Posted on April 1, 2021
People suffering from Lipoedema have often been mistaken as suffering from Lymphoedema or obese. My earlier blog entry “What is Lipoedema?” describes the condition briefly.
Please read a summary Bertsch 2020-Lipoedema – myths and facts, Part 5 (2020) by the European Lipoedema Forum consensus for more information. Here are some videos on patients with Lipoedema by Lipoedema UK (2019) and Channel Nine news 30 March 2021.
What is lymphoedema? FAQs on Lymphoedema and Cancer
Posted on March 1, 2021
March 2021 is Lymphoedema Awareness Month once again. There are books available via iTunes’ Apple Books covering Lymphoedema. There is one from Professor Peter Mortimer on Lets Talk Lymphoedema (2017). This time I would like to share my thoughts on a Book by Dr Teresa Lee ( a physiotherapist, NSW Australia).
Her E-book is available on Apple iBooks and Amazon.com.au and print copies available at navlymph.onlineweb.shop
Navigating Lymphoedema – A Guide for Cancer Survivors (2020 version)
Disclosure: I received a free digital copy of the book from the author. However, the comments are mine.
I would like to congratulate Teresa for taking on such a huge task of collating and writing up a much-needed resource tailored for cancer survivors with lymphoedema based in Australia, particularly for those with breast cancer. Teresa’s book is well-structured, logical, and comprehensive in coverage of the commonly asked topics. She covered each topic with the salient points in an unbiased concise easy-to-understand style. I particularly like the “Did you know” snippets that attempt to address points of debate or frequently asked questions.
Lymphoedema is not an easy condition to explain or write about and I feel this book is targeted towards people with a higher level of health literacy. Although there are pictures and illustrations throughout the book, I would have loved to see more to enhance the visual appeal. Interestingly, in a few instances, I feel that Teresa is sharing her thoughts one-on-one in detail with us as health professionals. Hence, this book may also be suitable for health professionals new to lymphoedema or who want to know more about the condition.
Overall, this is a value-for-money book that I would not hesitate to recommend to those clients who seek more in-depth information, education, and a sense of empowerment to navigate their lymphoedema journey. A labour of love, thank you Teresa for your effort.
Her E-book is available on Apple iBooks and Amazon.com.au and print copies available at navlymph.onlineweb.shop
Navigating Lymphoedema – A Guide for Cancer Survivors
Is it safe to receive COVID-19 vaccination when you have lymphoedema?
Posted on February 27, 2021
I had a query from my lymphoedema patient this week who was concerned about receiving her Covid-19 vaccination. So I thought it is timely to share a Consensus Document on Covid-19 Vaccination for patients with lymphoedema courtesy from UK. Specifically to acknowledge the experts’ work from the British Lymphology Society and The Lymphoedema Support Network.
This consensus document aimed to give advice regarding vaccination to patients with lymphoedema, based on the best available evidence and expert opinion.
Lymphoedema: Potential for Change
Posted on March 21, 2020

Weight loss and prescribed compression stockings
March is Lymphoedema Awareness Month. Thanks to Australian Physiotherapy Association (APA) for the chance for me (Linda Khong together with Christine Smith) to share some updates in APA InMotion with Lymphoedema: Potential for Change. Cancer-related lymphoedema only contributes to a small percentage of lymphoedema/chronic oedema cases worldwide. So what are the risk factors to chronic oedema or lymphoedema?
Introduction: Evidence has identified the cause and development of lymphoedema as a result of cancer treatment. In reality, cancer-related lymphoedema only contributes to a small percentage of lymphoedema cases worldwide. Improving awareness and an understanding of other chronic oedemas will contribute to improving outcomes for these patients. The information presented
in this article and the skills of physiotherapists can offer potential change for patients who consider their chronic oedemas as something they have to live with. If you prefer, download the PDF article with the reference list.
What may happen if I do nothing with my leg swelling?
Posted on December 14, 2019
This is the first paper of my research in lymphoedema conducted at one of Western Australia’s hospital with the help of a grant.
I feel privileged that the participants have taken the time to speak to me about their experience and the challenges they face. They are a group of 6 patients that have been disengaged or for several reasons refrained from management of their chronic swelling for over a decade. Basically, at this stage of research, I feel that their quality of life is abysmal and nearing disability. However, I am continuing with the analysis of the data. For those interested, please click on the following link.
Khong, LAM, Buckley A, Johnson W, Cavalheri, V. (2019). Lower limb chronic edema management program: Perspectives of disengaged patients on challenges, enablers and barriers to program attendance and adherence. PLoS ONE 14(11): e0219875. https://doi.org/10.1371/journal.pone.0219875
Can chronic swelling be treated?
Posted on November 17, 2019
Chronic oedema is a serious progressive medical disorder that should be treated promptly. This photo represents a typical case of of chronic swelling in the ankles and legs that have been left untreated for more than 10 years. It is probably due to longstanding incompetent leaky veins in the legs and repeated infections over time. Do you notice the discolouration, brown staining, change in skin condition (thick and dry) and overall enlargement of the legs and feet that developed? These changes makes day-to-day living challenging such as finding footwear that fits, walking and balance can become an issue.
The ‘after’ photo is the same patient’s leg after only 2 sessions within 6-weeks. There is reduced swelling and the skin looks better. The patient reported that her legs feel lighter so exercises and overall mobility has improved. Importantly, diuretics (water tablet) was not used to achieve this effect. Reach out to LK Lymphoedema Centre for a bespoke management approach suitable for you. Book an appointment online.
Should I use a compression pump? Self manage my lymphoedema?
Posted on October 27, 2019
This is a report from one of my client regarding use of her compression pump:
“I’ve had my compression pump for 12 months now and feel it is the best purchase I have made to self manage my lymphoedema. I didn’t get a health fund rebate on the actual pump but got 85% back on the leg sleeve. I am happy with what I spent when I compare that to the cost of having MLD done or even hiring the pump – it paid for itself in less than 6 months (compared to hiring).
I keep it next to my bed (with the leg sleeve and cables in a large basket) plugged in ready to go – no excuses! I do the half hour (per leg) massage 5-6 times a week wearing either a Mobiderm or Caresia garment for added benefit although it still does a good job without these. The massage it gives is quite firm but also relaxing and I either read or watch tv while its going on. I can feel it working down then up my leg similar to MLD and it works the back of my leg really well, which is a hard area to do yourself. I put my compression stockings on as soon as it is done.
As lymphoedema is a lifelong condition I accept that self management is the way to go (along with the guidance of a good therapist of course!) and this pump makes that easy to do. With continued regular use I feel my leg is a lot softer than it was and I see a marked improvement in the ankle and calf areas.”
Report on the Australia ILF-COM project
Posted on October 14, 2019
 This is a report by Dr Linda Khong as a follow-up to her participation (Australian) with the International Lymphoedema Framework- Chronic Oedema Outcome Measures (ILF-COM) project. Twelve frameworks involving 8014 people took part in the survey conducted December 2018 to end of March 2019. Each framework reported their respective ILF-COM findings via posters at the ILF Conference in Chicago 13-15 June 2019.
This is a report by Dr Linda Khong as a follow-up to her participation (Australian) with the International Lymphoedema Framework- Chronic Oedema Outcome Measures (ILF-COM) project. Twelve frameworks involving 8014 people took part in the survey conducted December 2018 to end of March 2019. Each framework reported their respective ILF-COM findings via posters at the ILF Conference in Chicago 13-15 June 2019.
Overall, the survey’s international respondents demonstrated that patients and healthcare professionals viewed limb volume, quality of life status and mobility status as three most important outcome measures as well deemed successful outcomes.
What causes chronic swelling?
Posted on October 10, 2019
There are many causes of leg swelling that is NOT due to Lymphoedema. Click here to read more about it from Mayo Clinic. Reasons for such swelling may arise from medications, being wheelchair bo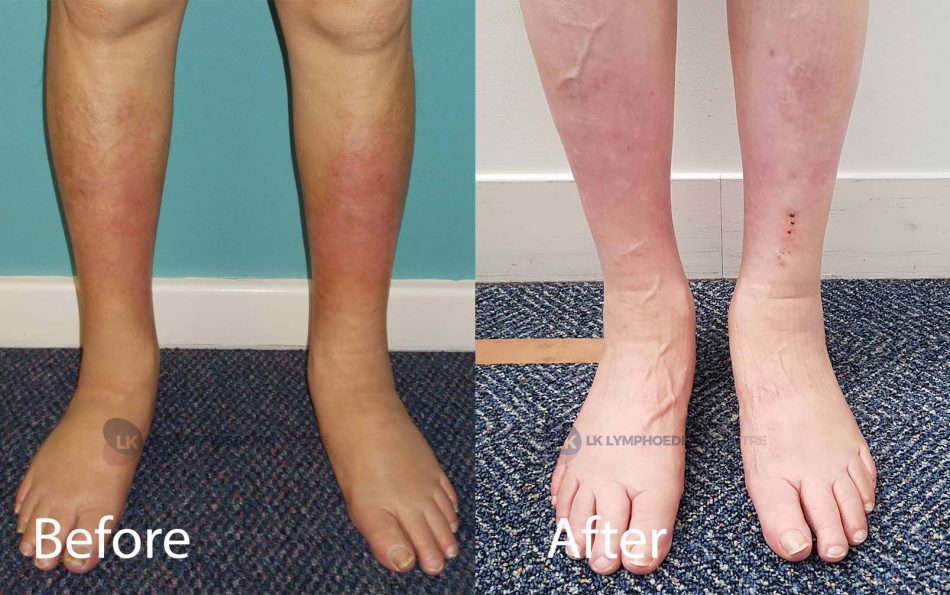 und, renal/cardiac issues and other reasons.
und, renal/cardiac issues and other reasons.
For example, this client (see photos included with permission) had persistent swelling in both legs, skin discolouration and repeated infections with skin tears a few years ago. The chronic swelling arose from several causes.
What do you think are the factors to successful effective oedema management in you case?
I have Type I diabetes and a history of renal failure with renal transplant in 2001. I have had vascular oedema of both legs for about 6 years or so. It has been exacerbated by antihypertensive (blood pressure) medications, in particular, calcium channel blockers.
The most important factor in managing my oedema has been the regular and consistent wearing of elastic stockings. Keeping on top of the swelling. This helps the swelling at bay and has improved the condition of my skin of lower limbs and no longer at risk of skin lesions and cellulitis.
Before photo was taken 1 year after regular treatment of CDT , stockings and more at the clinic.
After photo was taken 4 years later (2019). No more episodes of infections since treatment started, markedly reduced swelling and improved appearance. From the therapist’s perspective, the positive outcome can be attributed to thorough assessment cum management and the client’s positive attitude with sustained regular follow-up over time to manage the chronic condition.
It is important that you seek medical clearance first especially if you have swelling in both legs before booking an appointment with the clinic.













